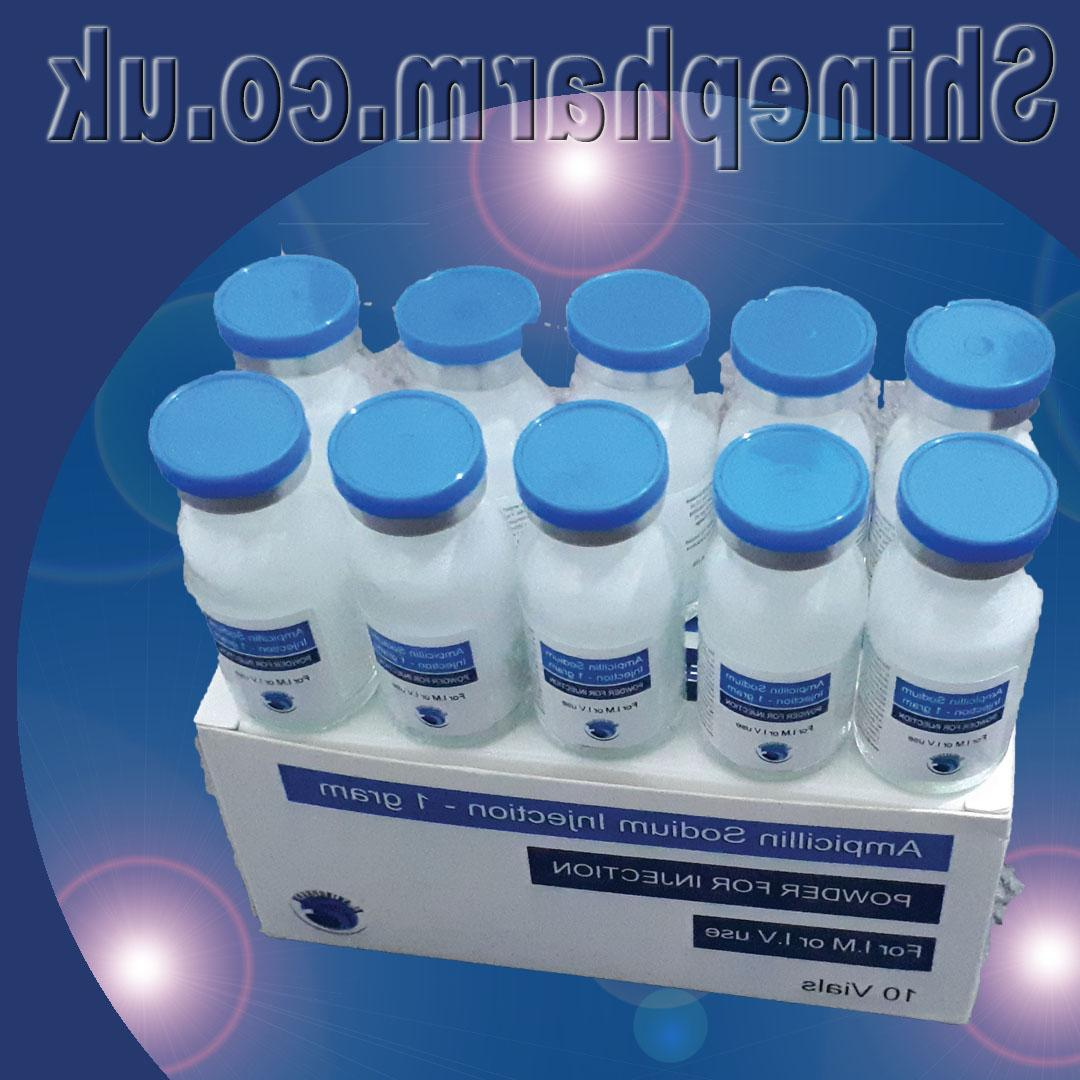
Ampicillin Injections



Ampicillin injections deliver broad-spectrum penicillin antibiotic activity through intravenous or intramuscular administration. These sterile formulations provide rapid bactericidal action against susceptible Gram-positive and Gram-negative organisms. Commonly used for serious infections like meningitis, septicemia, and endocarditis, ampicillin injections achieve higher and faster serum concentrations than oral forms. The medication works by inhibiting bacterial cell wall synthesis, particularly effective against Enterococci, Listeria, and E. coli. Hospital protocols typically dose every 4-6 hours based on infection severity and renal function. Proper aseptic technique is crucial for preparation and administration to maintain sterility.
Injectable ampicillin serves as first-line treatment for bacterial meningitis in neonates and Listeria infections in immunocompromised patients. Its spectrum covers common pathogens in intra-abdominal infections, UTIs, and respiratory tract infections when combined with beta-lactamase inhibitors. The injections are particularly valuable for treating enterococcal endocarditis (combined with aminoglycosides) and preventing Group B streptococcal infections during childbirth. Recent antimicrobial stewardship programs reserve ampicillin for specific indications due to rising resistance patterns. The injectable form is essential when rapid, reliable antibiotic levels are needed or when oral absorption is compromised.
Standard ampicillin injections come in 125mg/mL, 250mg/mL, and 500mg/mL concentrations. Adult dosing ranges from 250mg every 6 hours for mild infections to 2g every 4 hours for meningitis. Neonates receive 50-100mg/kg/day divided every 8-12 hours. IV administration requires reconstitution and dilution in compatible fluids (NS or D5W), infused over 10-30 minutes. IM injections use the ventrogluteal site for optimal absorption. Renal impairment mandates dose adjustment (CrCl <10mL/min: extend interval to 12-24 hours). Treatment duration typically spans 7-14 days depending on infection type and clinical response.
While oral ampicillin is suitable for mild outpatient infections, injections offer critical advantages in hospitalized patients. The IV/IM routes achieve therapeutic levels immediately versus 1-2 hour delay with oral capsules. Bioavailability is 100% with injections compared to 30-50% with oral forms due to gastric acid degradation. This makes injections essential for serious systemic infections, patients with vomiting/diarrhea, and those with absorption disorders. However, injections require clinical administration and carry higher risks of phlebitis or injection site reactions. Cost differences are modest, but injections incur additional preparation and administration expenses.
Common reactions include diarrhea (10-15% of patients), rash (5-10%), and thrombophlebitis at IV sites. Hypersensitivity reactions range from mild rashes to life-threatening anaphylaxis (1-3% of penicillin-naive patients). High doses may cause neurotoxicity (seizures) in renal impairment. Injection-specific risks include sterile abscesses at IM sites. Monitoring includes CBC (for leukopenia), renal function tests, and clinical response assessment. Patients should report severe diarrhea (possible C. difficile) or unusual bleeding/bruising. Contraindications include documented penicillin allergy and infectious mononucleosis due to high rash risk.
Pregnant patients (Category B) may receive ampicillin injections for indicated infections with fetal benefit typically outweighing risks. Neonatal dosing requires weight-based calculation and extended intervals in prematurity. Elderly patients need renal function assessment and potential dose reduction. Hemodialysis patients require supplemental dosing post-dialysis. Hepatic impairment doesn't require adjustment but necessitates extra monitoring for hypersensitivity. Patients with history of non-severe penicillin allergy may undergo supervised challenges when ampicillin is the optimal therapy.
Ampicillin exerts bactericidal effects by binding to penicillin-binding proteins, inhibiting transpeptidation in bacterial cell wall synthesis. Its extended spectrum compared to penicillin G includes improved activity against Gram-negatives like E. coli, Proteus mirabilis, and Haemophilus influenzae (non-beta-lactamase producers). The injections maintain efficacy against Enterococcus faecalis and Listeria monocytogenes - key pathogens in meningitis and endocarditis. Resistance develops via beta-lactamase production or altered PBPs. Unlike later-generation penicillins, ampicillin lacks stability against Staphylococcus aureus but remains a workhorse for susceptible Enterobacteriaceae in hospital and obstetric settings.
Approximately 40-60% of E. coli strains now show ampicillin resistance in community-acquired UTIs, necessitating pre-treatment cultures when possible. Hospital-acquired Enterobacterales resistance exceeds 80% in many regions. However, ampicillin retains reliable activity against Group B streptococci (98% susceptible) and Enterococci (85% susceptible for E. faecalis). Antimicrobial stewardship programs recommend reserving ampicillin for confirmed susceptible infections or specific clinical scenarios like neonatal sepsis. Rapid diagnostic methods like PCR have improved targeted use. Local antibiograms should guide empiric therapy decisions, with ampicillin remaining valuable in select cases despite broader resistance trends.
Reconstituted ampicillin maintains potency for 1 hour at room temperature or 8 hours refrigerated. IV solutions are stable for 24-48 hours depending on concentration and diluent. The medication is incompatible with aminoglycosides (must administer separately), vancomycin, and many electrolyte solutions. Pharmacy-prepared syringes for IM use remain stable for 3 days refrigerated. Proper technique requires thorough mixing until clear, avoiding vigorous shaking that causes foaming. Nursing staff should inspect for particulate matter or discoloration before administration. These handling requirements make ampicillin more labor-intensive than newer antibiotics but justify continued use for susceptible infections.
Generic ampicillin injections cost $5-$20 per gram, significantly less than broader-spectrum alternatives. Most hospital formularies maintain stock despite declining use due to its cost-effectiveness for susceptible infections. Insurance plans universally cover FDA-approved indications without prior authorization. Global health systems rely on ampicillin as an essential medicine for neonatal sepsis and obstetric infections. The low cost enables use in resource-limited settings, though increasing resistance threatens this advantage. Pharmacoeconomic analyses show ampicillin remains cost-effective for specific indications when guided by antimicrobial stewardship principles.
Current studies investigate ampicillin in combination with novel beta-lactamase inhibitors to overcome resistance. Research continues on optimized dosing regimens for obese patients and neonates using pharmacokinetic modeling. Investigational sustained-release IM formulations may allow less frequent dosing in outpatient parenteral antibiotic therapy. Microbiome research is clarifying ampicillin's ecological impact compared to broader-spectrum agents. These developments aim to preserve ampicillin's utility in an era of antimicrobial resistance while minimizing collateral damage to beneficial flora.
Patients receiving ampicillin injections require education about potential allergic reactions and the importance of completing the full course. Those transitioning to oral therapy should understand timing equivalencies. Diarrhea prevention strategies (probiotics, hydration) should be discussed. Women should be counseled about potential vaginal yeast infections. Patients must report severe diarrhea, rash, or swelling immediately. Discharge planning should address any needed follow-up cultures or laboratory monitoring. These points enhance safety and adherence during treatment.
Ampicillin injections are used for severe bacterial infections including: sepsis, meningitis, endocarditis, complicated UTIs, and respiratory infections caused by susceptible strains of E. coli, H. influenzae, and Streptococcus species. Particularly effective against Listeria monocytogenes.
• IV route preferred for serious infections (over 10-15 minutes)
• IM injection only for mild-moderate infections (deep into large muscle)
• Standard adult dose: 250-500mg every 6 hours
• Severe infections: Up to 2g every 4-6 hours IV
• Neonatal dosing: 50-100mg/kg/day divided q6-8h
Ampicillin vials require specific diluents (sterile water/NS) and proper technique to maintain sterility. Incompatible with dextrose solutions. Freshly prepared solutions must be used within 1 hour at room temperature or 24 hours if refrigerated.
1. Renal function (dose adjustment needed for CrCl <30ml/min)
2. CBC (may cause leukopenia/thrombocytopenia)
3. Neurological status (seizure risk at high doses)
4. Injection sites (thrombophlebitis risk with IV)
5. Diarrhea (may indicate C. difficile)
Ampicillin has: broader Gram-negative coverage than penicillin G, better CSF penetration (for meningitis), and is the preferred treatment for Enterococcus faecalis infections. However, it's inactivated by beta-lactamases.
• Epinephrine (for anaphylaxis)
• Antihistamines
• Corticosteroids
• Airway management tools
Ampicillin carries higher anaphylaxis risk than many antibiotics - test dose recommended for penicillin-allergic patients when essential.