Vitamin B12 Injections



Vitamin B12 injections deliver cobalamin directly into muscle tissue, bypassing digestive absorption barriers for patients with deficiencies. These intramuscular shots treat pernicious anemia, neurological disorders, and metabolic imbalances effectively. The therapy rapidly restores B12 levels, often showing improvements in energy and cognitive function within 48 hours. Standard protocols involve initial loading doses followed by maintenance therapy. Medical supervision ensures proper dosing to avoid potential side effects while monitoring hematological and neurological responses. Unlike oral supplements, injections guarantee 100% bioavailability, making them crucial for patients with intrinsic factor deficiency or malabsorption syndromes.
Injectable B12 offers distinct advantages for patients with absorption issues or severe deficiencies. The shots correct anemia faster than oral supplements, often normalizing blood counts within weeks. Neurological benefits include improved nerve conduction and reduced tingling sensations in extremities. Many patients report enhanced mental clarity and reduced fatigue after just 2-3 doses. The therapy also supports cardiovascular health by lowering homocysteine levels. Athletes use B12 injections for performance recovery, while older adults benefit from prevention of age-related cognitive decline. Properly administered injections avoid gastrointestinal absorption problems common with tablets.
Physicians prescribe B12 injections primarily for pernicious anemia and other malabsorption disorders like celiac disease or Crohn's. The treatment is standard for post-bariatric surgery patients and those with chronic atrophic gastritis. Neurological applications include diabetic neuropathy, multiple sclerosis symptom management, and Bell's palsy recovery. Emerging research explores benefits for depression, chronic fatigue syndrome, and fertility issues. Pediatric use addresses genetic disorders of B12 metabolism. Each condition requires specific dosing protocols, typically starting with frequent loading doses before transitioning to maintenance therapy.
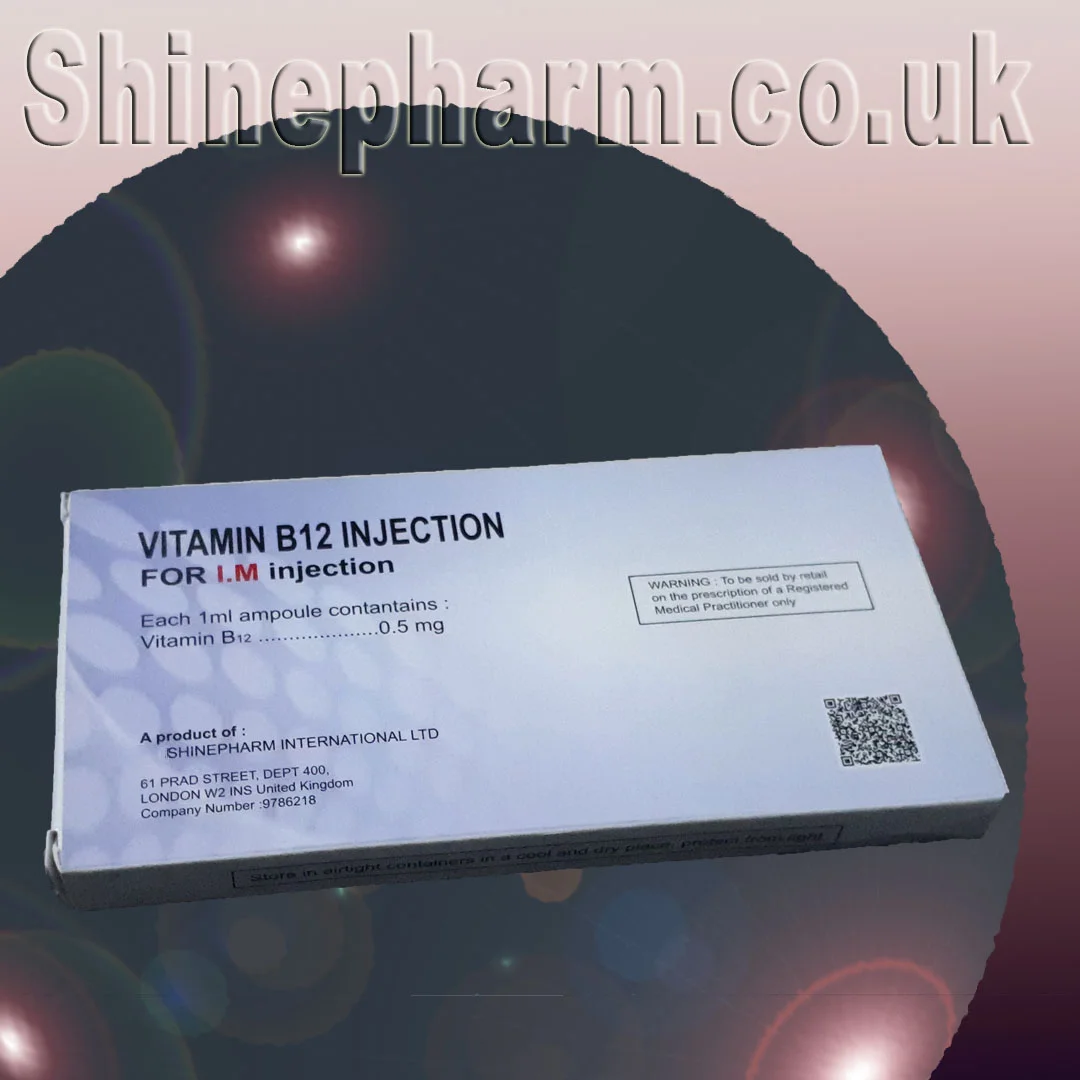
Standard B12 injections contain cyanocobalamin or methylcobalamin in 1000 mcg/mL concentrations. Initial treatment often involves 1000 mcg intramuscular injections daily for 7 days, then weekly for a month. Maintenance therapy typically requires monthly 1000 mcg doses. Subcutaneous administration is an alternative for self-injecting patients. The ventrogluteal or deltoid muscles are preferred injection sites. Recent protocols suggest methylcobalamin may offer better neurological outcomes. Treatment duration varies from temporary correction of deficiency to lifelong therapy for autoimmune pernicious anemia patients.
While oral B12 works for mild deficiencies, injections are essential for severe cases and absorption disorders. The injectable form achieves therapeutic levels immediately, whereas oral supplements require weeks of consistent dosing. Cost analysis shows injections are more economical long-term for chronic conditions despite higher upfront expenses. Patients with MTHFR gene mutations often respond better to certain injectable forms. However, injections require clinical visits or self-injection training. The choice depends on deficiency severity, underlying cause, and patient preference after thorough medical evaluation.
B12 injections are generally safe with minimal side effects when properly administered. Temporary reactions may include mild diarrhea, itching, or injection site discomfort. Rare but serious risks include anaphylaxis in cobalt-sensitive patients and hypokalemia during rapid blood cell production. Contraindications include Leber's disease and certain chemotherapy protocols. Drug interactions occur with metformin, proton pump inhibitors, and certain antibiotics. Regular monitoring of B12 levels, complete blood counts, and potassium levels ensures safe, effective treatment without complications.
Vitamin B12 injections work by directly replenishing depleted cobalamin stores, supporting two crucial enzymatic processes: methionine synthesis for nerve myelination and methylmalonyl-CoA conversion for energy production. The injections rapidly normalize homocysteine metabolism, reducing cardiovascular risks. Neurological benefits stem from restored myelin sheath integrity and improved nerve conduction velocity. Hematological improvements occur as B12 enables proper red blood cell maturation. Research shows injectable B12 achieves serum concentrations 40x higher than equivalent oral doses in deficient patients, explaining its superior clinical outcomes for severe cases.
Ideal candidates for B12 injections include patients with serum B12 levels below 200 pg/mL, elevated MMA or homocysteine, and clinical symptoms. High-risk groups include strict vegans, elderly individuals with atrophic gastritis, and patients with autoimmune disorders. Those experiencing neurological symptoms (tingling, balance issues) or hematological signs (macrocytic anemia) warrant immediate treatment. Diagnostic workup should rule out folate deficiency and include intrinsic factor antibody testing when appropriate. Asymptomatic patients with borderline levels may benefit from trial therapy if metabolic markers suggest functional deficiency.
Most patients notice energy improvements within 3-5 days, with hematological responses appearing by 2 weeks. Neurological symptoms may take 3-6 months to fully resolve. Initial intensive therapy (daily-weekly injections) typically lasts 1-2 months, followed by lifelong monthly maintenance for chronic conditions. Objective measures include regular CBC, reticulocyte counts, and neurological exams. About 5-10% of patients require adjusted dosing due to poor response, often from concurrent deficiencies or misdiagnosis. Follow-up testing ensures adequate treatment without overcorrection.
Generic B12 injections cost $10-$30 per vial, with administration fees adding $15-$50 per visit. Most insurance plans cover treatment for medically documented deficiencies, though frequency limits may apply. Medicare Part B covers injections for pernicious anemia with proper coding. Cash-paying patients can reduce costs by learning self-injection techniques. Price comparisons show injections are cost-effective versus high-dose oral therapy for chronic conditions when considering superior absorption and clinical outcomes.
Chronic B12 deficiency patients require indefinite therapy with regular monitoring. Maintenance schedules are individualized based on follow-up testing and symptom recurrence. Some patients transition to high-dose nasal sprays or sublingual forms after initial injection therapy. Dietary counseling helps vegetarian patients maximize B12 intake from fortified foods. Annual testing of B12, MMA, and homocysteine levels ensures ongoing treatment adequacy while preventing over-replacement. Patients are educated to recognize early deficiency symptoms for prompt retreatment.
Current studies explore ultra-high dose B12 injections for neurodegenerative diseases and autism spectrum disorder. New sustained-release formulations may allow quarterly dosing instead of monthly injections. Genetic research is identifying polymorphisms that predict superior response to specific B12 forms. Some clinics now offer personalized B12 protocols based on metabolic profiling. These advances promise to optimize treatment while reducing injection frequency for improved quality of life.
B12 injections are essential for: pernicious anemia (intrinsic factor deficiency), severe B12 deficiency (serum levels <200pg/mL), malabsorption disorders (celiac/Crohn's), post-gastrectomy patients, and certain neurological conditions (subacute combined degeneration). Also used for fatigue management in deficiency states.
• Cyanocobalamin: Synthetic form, requires conversion to active B12, longer shelf life, lower cost
• Methylcobalamin: Bioactive form, immediate utilization, preferred for neurological symptoms, more expensive
• Hydroxocobalamin: Used for cyanide poisoning, longest-acting
• Standard dose: 1000mcg/ml
• Routes: Deep IM (gluteal/deltoid) or subQ (abdominal)
• Loading phase: Daily/weekly for 1-4 weeks
• Maintenance: Monthly or every 3 months (hydroxocobalamin)
• No need for aspiration before injection
Oral absorption requires intrinsic factor (absent in pernicious anemia) and healthy ileum. Injections bypass these requirements, providing 100% bioavailability regardless of GI function. Only 1% of oral B12 is absorbed passively without intrinsic factor.
Yes - with proper training. Subcutaneous administration is simpler for self-injection. Prefilled syringes and auto-injectors are available. Must rotate sites and monitor for lipohypertrophy with long-term use.
1. Contraindicated in Leber's disease (hereditary optic neuropathy)
2. May cause hypokalemia during initial treatment (monitor potassium)
3. Risk of false-normal B12 levels after recent injection
4. Can mask folate deficiency
5. Allergy risk to cobalt or preservatives (rare)
• Energy improvement: 24-72 hours
• Reticulocyte response: 3-5 days
• Neurological improvement: Weeks to months
• Hematological normalization: 4-8 weeks
• Maximum nerve repair: Up to 1 year
• Injection site reactions (15-20%)
• Mild diarrhea (initial doses)
• Itching/eczema (cobalt sensitivity)
• Transient anxiety (overstimulation)
• Headache (usually resolves quickly)
Serious reactions are extremely rare.
• Baseline: CBC, B12, folate, iron studies
• Repeat B12 levels 1 month after loading dose
• Annual checks for chronic therapy
• Monitor potassium during initial treatment
• Neurological exams for neuropathic symptoms
B12 injections can "mask" megaloblastic anemia from folate deficiency while allowing neurological damage to progress. Always assess both vitamins before initiating therapy.